by Toug Tanavin, MD, Mark Pollet, MD,
and Yochai Birnbaum, MD, FACC
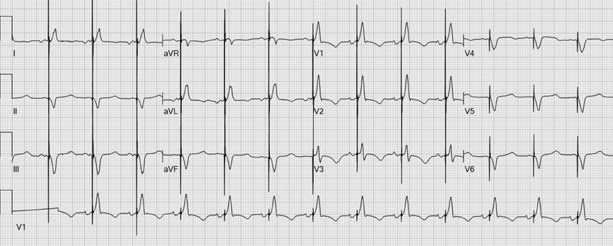
A 61-year-old man with coronary artery
disease presented with volume overload caused by medication noncompliance. His
medical history included percutaneous coronary intervention; ischemic
cardiomyopathy (left ventricular [LV] ejection fraction, <0.15); and
placement of a biventricular implantable cardioverter-defibrillator (ICD),
model and programming unknown. Chest radiographs showed properly positioned
ventricular and right atrial leads. Figure 1 shows the patient’s
electrocardiogram (ECG) on presentation.
On the
basis of the ECG, what is the patient’s diagnosis?
A) Supraventricular
tachycardia with biventricular pacing response
B) Pacemaker-mediated
tachycardia
C) Sinus
tachycardia with normal atrioventricular delay programming
D) Antitachycardia
pacing
Answer
A) Supraventricular
tachycardia with biventricular pacing response
The ECG shows a relatively narrow QRS
complex at a ventricular rate of 100 beats/min. Notably, an rSR' configuration
in leads V1 and V2 (Fig. 2A, arrows) represents a
retrograde P wave that suggests supraventricular tachycardia—most likely
atrioventricular nodal reentry tachycardia, not sinus tachycardia with normal atrioventricular
delay programming.1 The ventricular pacemaker stimuli after each
intrinsic QRS complex are probably from responsive biventricular ICD pacing. After
the patient’s tachycardia resolved, we observed sinus rhythm, normal right
bundle branch configuration, and normal biventricular pacing (Fig. 2B).
 |
| Fig. 2A |
 |
| Fig. 2B |
When the ICD senses intrinsic activity
in one ventricle, it immediately paces the other ventricle, to better synchronize
LV contraction. However, the initially narrower QRS configuration suggests that
the LV pacing stimuli were not capturing the already depolarized ventricular
myocardium. Responsive biventricular ICD pacing is expected to produce fusion
complex morphology, as in cardiac resynchronization therapy, and indeed the
wider QRS complex after conversion to sinus rhythm indicates fusion from
His–Purkinje system depolarization with coinciding pacing stimuli.
In Figure 1, the response is not
antitachycardia pacing, because the pacing stimuli occur before the QRS complexes;
moreover, there was no burst of pacing stimuli faster than the spontaneous
rate.1 Nor is the response pacemaker-mediated tachycardia, because
the pacing stimuli occur after the QRS complexes begin.2,3 The P
waves at the end of the QRS complexes might be retrograde conduction from the
pacemaker stimulus; however, the very long subsequent PR intervals suggest another
mechanism.
References
- Issa ZF, Miller JM, Zipes DP. Clinical arrhythmology and electrophysiology: a companion to Braunwald’s heart disease. 2nd ed. Philadelphia: Elsevier Saunders; 2012. p. 381-410.
- Cha YM, Mulpuru SK. Cardiac resynchronization therapy programming and troubleshooting. In: Ellenbogen KA, Wilkoff BL, Kay GN, Lau CP, Auricchio A, editors. Clinical cardiac pacing, defibrillation, and resynchronization therapy. 5th ed. Philadelphia: Elsevier; 2017. p. 1090-132.
- Burri H. Pacemaker programming and troubleshooting. In: Ellenbogen KA, Wilkoff BL, Kay GN, Lau CP, Auricchio A, editors. Clinical cardiac pacing, defibrillation, and resynchronization therapy. 5th ed. Philadelphia: Elsevier; 2017. p. 1031-63.


No comments:
New comments are not allowed.